Pressure Injuries: Early Signs, Prevention, and Treatment
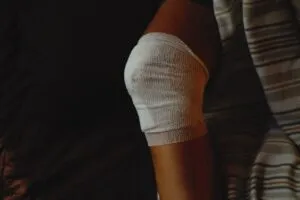
Pressure injuries, also known as bedsores, develop when prolonged pressure restricts blood flow to certain areas of the skin. These injuries can be painful, slow to heal, and lead to serious infections. Early detection is critical to preventing severe complications.
Do you notice red or discolored areas on your skin that don’t fade after relieving pressure? Are there patches of skin that feel warmer or cooler than the surrounding areas? These may be the first signs of a pressure injury. According to prevention strategies, including frequent movement and skin assessments, are essential for avoiding severe wounds.
Pressure injuries can develop quickly, especially in individuals with limited mobility. The risk is even higher for those with conditions like diabetes, poor circulation, or malnutrition. Without proper care, these wounds can progress, leading to open sores, infections, and in extreme cases, deep tissue damage. The OECD’s health research emphasizes the importance of early intervention in reducing healthcare burdens associated with chronic wounds.
Video Component Placeholder
The Role of Wound Assessment in Pressure Injury Treatment
Wound assessment plays a pivotal role in managing pressure injuries. It helps healthcare professionals determine the severity of the wound and tailor treatment plans accordingly.
Key Steps in Wound Assessment
- Identifying the Stage of the Wound: Pressure injuries range from mild (Stage 1) to severe (Stage 4), where the damage extends to the muscle and bone.
- Measuring Wound Size and Depth: Tracking wound dimensions over time helps gauge healing progress.
- Assessing Wound Bed Condition: The presence of necrotic tissue, slough, or granulation tissue determines the next course of action.
- Monitoring Signs of Infection: Redness, swelling, or foul odor can indicate bacterial infection requiring urgent treatment.
Proper assessment ensures that treatments like negative pressure wound therapy, which has been explored in this in-depth analysis, are implemented effectively.
Preventative Strategies for Pressure Injury Treatment
Preventing pressure injuries is always better than treating them. Implementing a few simple strategies can drastically reduce the risk of developing bedsores.
1. Regular Repositioning
Frequent movement relieves pressure on vulnerable areas. Patients should shift positions every 1-2 hours in bed and every 15 minutes if seated.
2. Specialized Support Surfaces
Pressure-relieving mattresses, cushions, and overlays distribute weight evenly, reducing pressure buildup on bony prominences.
3. Skin Care and Hygiene
- Keep the skin clean and moisturized to prevent dryness and irritation.
- Use mild, pH-balanced cleansers.
- Apply barrier creams to protect against moisture-associated skin damage.
4. Nutrition and Hydration
- A protein-rich diet supports tissue repair.
- Vitamin C and zinc boost collagen production and immune response.
- Adequate hydration prevents skin breakdown and promotes circulation.
Advanced Pressure Injury Treatment Methods
When pressure injuries become severe, advanced treatment approaches are necessary.
Debridement: Removing Dead Tissue
Necrotic tissue can slow healing and increase the risk of infection. Medical professionals use sharp, enzymatic, or autolytic debridement methods to clear away dead tissue.
Negative Pressure Wound Therapy (NPWT)
NPWT uses a vacuum-assisted system to promote wound healing by:
- Reducing excess fluid and swelling
- Increasing blood circulation
- Encouraging new tissue growth
Discover more about how NPWT accelerates wound recovery in our detailed breakdown on innovations in negative pressure wound therapy.
Skin Grafts and Flap Surgery
For deep pressure injuries, surgical interventions may be necessary. Skin grafts involve transplanting healthy skin to cover the wound, while flap surgery uses nearby tissue to close large wounds.
Antibiotic Therapy and Infection Control
Infected wounds require targeted antibiotic treatment to prevent systemic complications. Regular wound cleaning and specialized dressings help minimize bacterial growth.
When to Seek Professional Care for Bed Sore Treatment

Understanding Bed Sores and Their Severity
Bed sores, also known as pressure ulcers or pressure injuries, develop when prolonged pressure on the skin reduces blood flow to the affected area. These wounds most commonly occur in individuals who have limited mobility, such as bedridden patients or those in wheelchairs. While some minor pressure injuries can be managed at home, others require professional intervention to prevent serious complications, including infections and tissue death.
Signs That You Need Professional Bed Sore Treatment
Some pressure injuries may seem manageable at first, but certain warning signs indicate the need for immediate medical attention. If you notice any of the following symptoms, it’s time to seek expert wound care.
1. Persistent Redness or Pain That Does Not Improve
If a pressure ulcer remains red, irritated, or painful despite repositioning and proper at-home wound care, it may indicate ongoing tissue damage. Persistent redness is often a sign of early-stage bed sores that are not healing as expected, requiring medical evaluation.
2. Open Sores, Pus Drainage, or Foul-Smelling Wounds
When a pressure ulcer progresses to an open wound, it becomes highly susceptible to bacterial infections. The presence of pus, increased drainage, or a foul odor suggests an infection that could spread if left untreated. In such cases, professional wound care specialists can provide advanced dressings, debridement, and antimicrobial treatments to promote healing.
3. Signs of Tissue Necrosis (Blackened Skin or Dead Tissue)
Bed sores that exhibit black, brown, or darkened skin indicate tissue death (necrosis). This can lead to further complications, including gangrene and sepsis if not addressed promptly. Specialized wound debridement and surgical intervention may be necessary to remove dead tissue and promote new cell growth.
4. Fever or Chills Indicating Infection
A fever, chills, or other systemic symptoms such as increased heart rate and confusion may indicate that an infection has spread beyond the wound site. This is a medical emergency requiring immediate intervention to prevent conditions like sepsis, which can be life-threatening.
5. Slow or No Improvement Despite Home Care
If a bed sore does not show noticeable improvement within a few weeks of diligent wound care, it may require professional treatment. Delayed healing can be due to underlying conditions such as diabetes, poor circulation, or inadequate nutrition, all of which should be assessed by a wound care specialist.
The Importance of Early Professional Intervention
Seeking professional care for pressure injuries at the right time can prevent complications and speed up recovery. At Optimum Wound Care Center (OWC Center), our expert team provides:
- Comprehensive Wound Assessment: Identifying the stage of the bed sore and the best treatment approach.
- Advanced Wound Dressings: Specialized dressings that promote healing and reduce infection risk.
- Debridement Therapy: Safe removal of dead or infected tissue to support new cell growth.
- Infection Management: Antibiotic therapy and infection control measures for wound healing.
- Personalized Pressure Injury Treatment Plans: Tailored strategies to prevent recurrence and promote long-term skin health.
Pressure injuries, or bedsores, are a serious concern, particularly for individuals with limited mobility. Recognizing the early signs—such as persistent redness, temperature changes in the skin, and discomfort—can prevent minor irritations from escalating into severe wounds. Simple preventative measures like frequent repositioning, maintaining skin integrity, and ensuring proper nutrition play a crucial role in reducing risk.
For those already dealing with pressure injuries, timely intervention is key. Treatments range from debridement to remove dead tissue, negative pressure wound therapy to accelerate healing, and, in severe cases, surgical procedures like skin grafts. Infection control remains a top priority, as untreated wounds can lead to significant complications.
Caregivers are instrumental in both prevention and treatment, assisting with movement, monitoring skin health, and ensuring proper nutrition. When pressure injuries persist despite home care efforts, seeking professional wound care is essential. With specialized treatment options and expert guidance, recovery becomes more achievable, preventing further complications and improving overall well-being.
Key Takeaways
- Early Detection Prevents Severe Pressure Injuries
Recognizing the first signs of a pressure injury—such as persistent redness, temperature changes, or skin discomfort—can prevent serious complications. Regular skin inspections and early intervention can significantly reduce the risk of developing severe wounds.. - Frequent Repositioning and Support Surfaces Reduce Risk
Shifting positions regularly and using specialized support surfaces, such as pressure-relieving mattresses and cushions, help distribute weight and minimize prolonged pressure on vulnerable areas. These simple adjustments are crucial for preventing pressure injuries, especially in individuals with limited mobility.. - Nutrition and Hydration Play a Vital Role in Wound Healing
A well-balanced diet rich in protein, vitamin C, and zinc helps maintain skin integrity and supports faster wound healing. Hydration is equally important, as it improves circulation and prevents skin breakdown. Proper nutrition strengthens the body’s ability to recover from wounds effectively. - Advanced Treatments Accelerate Healing for Severe Cases
When pressure injuries progress to advanced stages, medical interventions like negative pressure wound therapy (NPWT), debridement, and skin grafts may be necessary. These treatments promote healing, remove necrotic tissue, and restore damaged skin.
5. Professional Wound Care is Essential for Complex Cases
If a pressure injury worsens or shows signs of infection—such as pus, swelling, or tissue necrosis—seeking expert medical care is crucial. OWC Center provides comprehensive wound care solutions, from advanced therapies to customized treatment plans, ensuring optimal recovery.
Related Questions Asked and Answered
1. What are the best ways to prevent bed sores?
Preventing bed sores requires a combination of lifestyle adjustments and medical interventions:
- Frequent Repositioning: Shift positions every 1-2 hours.
- Skin Inspections: Regular checks for early signs of pressure injuries.
- Nutrition and Hydration: Proper intake of protein and vitamins for skin integrity.
- Specialized Support Surfaces: Pressure-relieving cushions and mattresses.
- Skincare Routine: Moisturizing and keeping skin clean to reduce friction.
2. How can caregivers help with pressure injury prevention?
Caregivers play a vital role in pressure injury prevention by:
- Assisting with Position Changes: Ensuring patients move frequently.
- Encouraging Mobility: When possible, promoting light movement.
- Maintaining Skin Health: Keeping the skin dry and moisturized.
- Monitoring Nutrition: Providing nutrient-rich meals and adequate hydration.
- Performing Regular Wound Assessments: Checking for early signs and reporting changes.
3. What treatments are available for severe pressure injuries?
Advanced pressure injuries require specialized care, including:
- Debridement: Removing dead tissue.
- Negative Pressure Wound Therapy (NPWT): Speeds up healing with vacuum-assisted therapy.
- Skin Grafts and Surgery: In extreme cases, reconstructive procedures may be necessary.
- Infection Control: Antibiotics and specialized wound dressings prevent complications.
For professional pressure injury treatment, consult with our wound care specialists.
4. How does nutrition affect wound healing?
Proper nutrition is critical for wound healing:
- Protein: Essential for tissue repair.
- Vitamin C and Zinc: Promote collagen production and immune function.
- Hydration: Prevents skin dryness and improves circulation.
A balanced diet can accelerate recovery and prevent further complications.
5. When should I seek medical attention for a pressure injury?
Seek medical care if you notice:
- Persistent Redness or Pain: Skin irritation that does not improve.
- Open Wounds or Pus Drainage: Signs of infection.
- Tissue Necrosis: Blackened or dead tissue.
- Unexplained Fever: Possible systemic infection.


